Choose the alternative so as to have the poem completed correctly.
In “Believe that as long as you believe in yourself – anything is possible”, the underlined expression is used to talk about
The aging process affects us all at different rates. Some people
of fifty-three, like the esteemed author, look a mere thirty-five, with
sparkling brown eyes, a handsome gait and the virility of a steam train.
Others, like the author's friend Colin, look like little middle-aged men
at twenty-one with middle-aged outlooks of set ways and planned
futures. In women the former condition is common but women rarely
suffer from the latter, being fired with the insatiable drive of ambition
for either an independent and distinguished career in a still
male-dominated world, or a home and seven children by the time they
are thirty followed by an independent and distinguished career as a
Cheltenham councillor or a public relations agent for Jonathan Cape, in
later life.
No such luck for Charles Charlesworth, who was born on the
14th of March, 1829, in Stafford. At the age of four Charles had a beard
and was sexually active.
In the final three years of his life his skin wrinkled, he
developed varicose veins, shortness of breath, grey hair, senile dementia
and incontinence. Some time in his seventh year he fainted and never
gained consciousness.
The coroner returned a verdict of natural causes due to old age.
Hugh Cory. Advanced writing with english in use. Oxford University Press, p. 34
According to the text above,
women around 30 have had distinguished careers in spite of living in a male-dominated world.
This text refers to questions from 39 to 41
There are very broad trends that affect almost all industries
and we can see them manifest in specific ways in each industry.
Generally, there is, as if it were, a kind of a "perfect storm"
gathering. With the more widespread adoption of the Internet, more
and more users are turning to it for e-commerce, trading,
reservations, gambling, and so on. This in turn increases the
numbers of transaction and information processing that need to be
conducted in near-real-time. In addition, organizations are using
more and more real-time systems to analyze information on-the-fly
and make automated decisions based on this information analysis
in real time. This is also becoming feasible because of the
significant reductions in the cost of computing infrastructure:
powerful machines based on commodity x86 architectures, open
source operating systems (Linux, Solaris), etc. With grid
technologies (such as GigaSpaces), they can aggregate these
machines into powerful computer systems previously only possible
with expensive mainframes and proprietary SMP machines.
Internet: (adapted).
In the text, “In addition” means
Read the paragraph below to choose the alternative that
best summarizes it.
“Understanding these dominant traditions within the logic
of the multicultural suggests the need for coalitions and coproduction
in knowledge formation which takes seriously the
“local memories” and “subjugated knowledge” (according to
Foucault) whose exclusion and repression shore up the
dominant tradition as an unquestionably valorized (western)
universal foundation.”
Choose the alternative that best transforms into reported
speech what is said in the cartoon below.
Read the sentences below.
I. Teachers have been meeting in the coffee shop.
II. Text-books were growing smaller.
III. Will the school board have finished their reports by
Wednesday?
IV. Students haven’t written their essays on American
literature.
Choose the alternative that indicates the verb tenses used
in the sentences, respectively.
Read the sentence below and choose the alternative that
fills in correctly the blank.
The Titanic, sunk in 1912, has been the subject of
numerous films and books, __________?
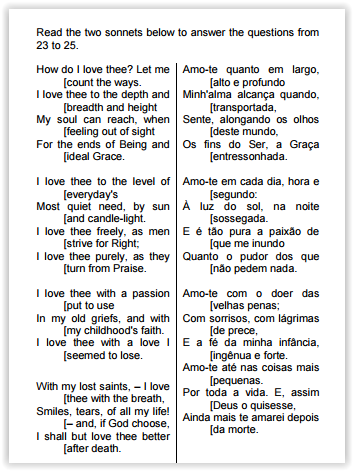
As you have seen above, the Brazilian poet Manuel Bandeira translated Sonnet 43 into Portuguese. About his translation, it’s correct to say that it’s
THERE ARE 5 QUESTIONS OF MULTIPLE CHOICE IN YOUR TEST. EACH QUESTION HAS 4
ALTERNATIVES (A, B, C, AND D) FROM WHICH ONLY ONE IS CORRECT. CHECK THE CORRECT
ONE.
Don't Get Sick in July
By Theresa Brown
Published: July 15, 2012
It's one of those secrets you normally don't learn in nursing school: ''Don't go to the hospital in
July.'' That's the month when medical residents, newly graduated from medical school, start learning how
to be doctors, and they learn by taking care of patients. And learning means making mistakes.
There's disagreement in the medical literature about whether a so-called July Effect, where
medical error rates increase in the summer, actually exists. But a 2010 article in the Journal of General
Internal Medicine and a 2011 article in the Annals of Internal Medicine both found evidence of it. In an
interview, Dr. John Q. Young, lead author of the latter review, likened the deployment of new residents to
having rookies replace seasoned football players during ''a high-stakes game, and in the middle of that
final drive.''
From what I've experienced as a clinical nurse, whether or not the July Effect is statistically
validated as a cause of fatal hospital errors, it is undeniably real in terms of adequacy and quality of care
delivery. Any nurse who has worked in a teaching hospital is likely to have found July an especially
difficult month because, returning to Dr. Young's football metaphor, the first-year residents are calling the
plays, but they have little real knowledge of the game.
This experience deficit plays out in ways large and small, but I remember an especially fraught
situation one July when a new resident simply did not know enough to do his job and a patient quite
literally suffered as a result.
The patient was actively dying. He was old and his death was expected. He had kept his cancer
at bay for several years, but there were no more curative treatment options left and he had opted to die
peacefully in his bed, surrounded by his family. He had also wanted to die in the hospital, and his death
was coming on quickly enough that the hospital decided to allow it. He was grumpy, charming, funny and
impressively clear-eyed about the end of his life. During our brief, two-day acquaintance I developed a
strong attachment to him.
Death came closer quickly on that second day and as it neared, his pain increased significantly.
Dying from cancer often hurts. He needed oxygen to breathe comfortably, and because he was alert he
fully felt the intense pain.
I'm a nurse, so legally I cannot decide to increase a patient's dose of pain medication, but I can
call a physician and describe the patient's distress. That's part of a nurse's job, but there is also a chain
of command for getting medication orders, and another part of my job is adhering to that hierarchy.
I paged the first-year resident covering the patient. Since it was July he was an M.D. on the
books, but he was brand new to actual doctoring. I explained things, but he would not increase the
ordered dose. I paged him again. We talked over the phone, and I insisted. Then I pleaded. He would
not up the dose.
Looking at the situation from his point of view, I understand his reluctance. I was asking him to
prescribe a very large dose of narcotic, a killingly big dose if the patient was unused to opioids. The
resident might have learned in medical school about pain during dying, but he had not actually been with
a patient going through it. Seeing such pain -- the body twisting, the patient crying out helplessly -- is
categorically different from reading about it.
I also imagine the resident had been taught to prescribe narcotics judiciously, perhaps even
sparingly, and the amount of drug I was asking for was neither.
The patient's wife was kind; his daughter, a nurse, forthright. They and he deserved better than
they were getting, so I decided to take a risk. Ignoring the chain of command, I paged the palliative care
physician on call. She and I had talked about the patient the day before.
I described the patient's sudden lurch toward death, the sharp increase in pain and the resident's
reluctance to medicate the patient enough to give him relief. ''Ah,'' she said, ''I was worried about that,''
meaning that the patient might begin actively dying sooner than the medical team had expected. She
ordered a morphine pump. I got the drug, loaded and programmed the machine. The patient died fairly
soon after. He was conscious to the very end, and I can say he did not meet his death in agonizing pain.
A few hours later I ended up in the elevator with the new resident. He and I both started talking at
once. Looking stricken, he apologized to me for having been busy, overwhelmed with several new
patients. Knowing it is never easy to have someone's footprint on your head, I apologized for having
called in an attending physician. ''I don't usually jump the line,'' I started to explain, when he interrupted
me. ''You did the right thing for the patient,'' he said.
Such an exchange is rare. A nurse who goes over a doctor's head because she finds his care
decisions inappropriate risks a charge of insubordination. A resident who doesn't deliver good care risks
the derision of the nurse caring for that patient. Nurses aren't typically consulted about care decisions,
and this expectation of silence may lead them to lash out at doctors they see as inadequate.
The July Effect brings into sharp relief a reality of hospital care: care is becoming more
specialized, and nurses, who sometimes have years of experience, often know more than the greenest
physicians. We know about medicating dying patients for pain, but we know a lot of other things, too:
appropriate dosages for all kinds of drugs, when transfusions and electrolyte replacements are needed,
which lab tests to order and how to order them, whether consulting another specialist is a good idea,
whether a patient needs to go to intensive care because his vital signs are worryingly unstable.
The problem can be limited by better supervision from senior residents, fellows and attending
physicians, as well as by nurses. We need to acknowledge this fact, because admitting that new
residents need help, and that nurses can and do help them, is the beginning of owning up to our shared
responsibilities in providing care. For the good of our patients, nurses and doctors need to collaborate.
(http://query.nytimes.com/gst/fullpage.html?res=9C02E3DB143FF936A25754C0A9649D8B63&ref=nursingandnurses)
The word underlined in this passage of the text “I'm a nurse, so legally I cannot decide to increase a patient's dose of pain medication” means
Choose the correct sentence, as far as the use of another/other/others is concerned.
Complete the sentences with the correct reflexive
pronouns.
1- The fashion models had a great vacation. They
enjoyed __________ very much.
2- Michael has cut ____________ in the laboratory.
3- Lucy told me ____________ that the Spanish
teacher was sick.
4- Be careful. The water is very hot. Don't burn
________________.
Choose the option that provides the correct pronouns
that complete the sentences above, respectively.